
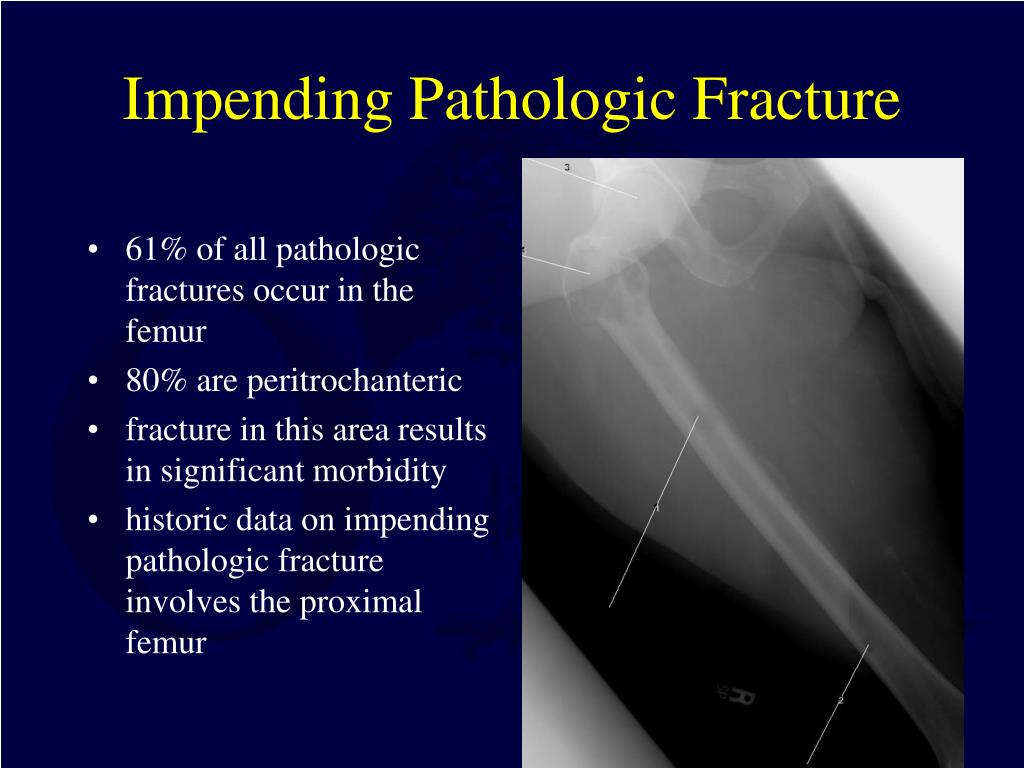
In response to this, we sought to develop a novel scoring system based on the statistically significant variables identified at the time of pathological fracture that can be utilised to more accurately predict prognosis and overall survival. Īlthough important, the documented ability of clinicians to predict prognosis in patients with metastatic bone disease is poor, with reported accuracy of only 18% reported in the literature. The chosen implant and construct should be able to withstand the patient’s expected level of activity and appropriately match their expected survival. When considering surgical management of a pathological fracture, the key operative goals include pain relief, early mobilisation and minimal morbidity and complications. However, this study differs by identifying the significant variables at time of pathological fracture, which is often the point at which the surgical team are first involved. Ī number of studies have identified significant variables in patients with metastatic lesions and how they relate to patient prognosis. The literature suggests a 1-year survival rate in the range of 30–40%. Pathological fractures have significant implications for patient morbidity and mortality and are often considered a marker of end-stage cancer. Approximately 10% of patients with bony metastases will suffer a pathological fracture at some point during their clinical course. Recent advances in diagnostic and therapeutic capabilities have resulted in a better prognosis in many cancer patients. This can guide specialist management and offer patients a more accurate expectation of functional outcome and survival time.Īs the average life expectancy has increased, so too has the prevalence of cancer.
ConclusionĪ novel scoring system has been developed that offers a survival probability based on patient’s individual circumstances. There was a statistically significant association between patient survival and primary cancer type, physical functional score, spinal metastatic burden and use of chemotherapy or radiotherapy. Median time from cancer diagnosis to pathological fracture was 14.2 months.
Median survival from fracture to death was 4.1 months. ResultsĪ total of 233 patients were included. Variables assessed were primary cancer type, fracture site, fixation method, cement augmentation, pre-morbid level of physical functioning, complication rate, treatment with chemotherapy or radiotherapy and appendicular, spinal and visceral metastatic load. The records of all patients that presented with metastatic pathological fractures over a 10-year period from the only tertiary orthopaedic departments in Western Australia were retrospectively examined. The aim of this study was to identify the variables that influence prognosis and utilise these to develop a novel scoring system to better predict life expectancy post-pathological fracture. The most appropriate treatment of pathological fractures from metastatic disease depends on several factors, one of the most important being predicted life expectancy.


 0 kommentar(er)
0 kommentar(er)
